Introduction:
The routine incorporation of proteasome inhibitors, immunomodulatory drugs (IMIDs), and monoclonal antibody drugs (mAbs) in managing multiple myeloma (MM) has improved patients' prognosis. Unfortunately, triple refractory patients continue to do poorly. Immunotherapeutic approaches (mAbs, CAR-T cells) have shown the most promise in these patients. However, the efficacy of these therapies depends on a functional tumor immune microenvironment (iTME), which is extensively reshaped by existing MM therapies and disease evolution. Understanding how the iTME and malignant clone co-evolve over the disease course is crucial to optimize the use of immune-based treatments and understand their mechanisms of action.
Methods:
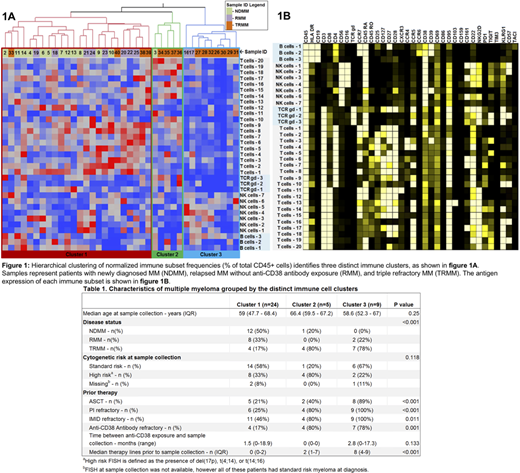
Newly diagnosed MM patients (NDMM), MM patients relapsing prior to anti-CD38 antibody exposure (RMM), and triple refractory MM patients (TRMM) were identified from the Mayo Clinic biospecimen database. We performed CyTOF (with a 37 marker lymphoid panel on CD138- bone marrow [BM] mononuclear cell samples) to assess the cellular iTME, Luminex (using BM plasma) to assess the humoral iTME (cytokines and chemokines) and RNAseq analysis (using BM CD138+ cells) to assess the malignant clone transcriptome. Astrolabe was used to identify immune cell clusters. Gene set enrichment analysis (GSEA) was used to identify gene pathways with differential expression across groups. JMP was used to perform unsupervised hierarchical clustering and descriptive statistics. An FDR corrected p value of <0.05 was considered statistically significant for all comparisons.
Results:
This study included 39 patients (13 NDMM, 11 RMM, and 15 TRMM). Samples were hierarchically clustered by cellular iTME, humoral iTME and malignant cell transcriptome, separately. The cellular iTME best recapitulated known disease biology and was used as the "anchoring" variable for subsequent analyses. Three distinct immune clusters were identified (figure 1): cluster 1, comprised mainly of NDMM and RMM patients; and clusters 2 and 3, comprised primarily of TRMM patients. In cluster 2, 4/5 patient samples were collected immediately after progression on daratumumab-IMID therapy, whereas all 7 TRMM patient samples in cluster 3 were collected at a median of 2.8 (range 0-17.2) months after last daratumumab exposure (table 1).
Most naïve T cell subsets (including the TIGIT+ T5 and the C38/CD127+ subsets T1, T2, and T12) were highest in cluster 1 compared to clusters 2 and 3. Several unfavorable T cell subsets were elevated in Cluster 2: 1) CD161+ T6, T7 and T17 subsets, which are thought to be Th17 polarized cells that promote MM growth; 2) T7, T9 CCR5+ subsets, which are thought to represent tumor-specific exhausted (PD-1+) T cell subsets; 3) senescent subsets (T-10, T14, T16,T18, T19); and 4) TCR-gd subsets with features of senescence (KLR, CD57), exhaustion (PD-1, TIGIT) and Th17 polarization (CD161).
There were no significant differences in cytokine and chemokine expression based on disease status (NDMM, RMM, or TRMM) or iTME (immune clusters 1, 2, or 3). GSEA was performed to compare clusters 2 and 3 (TRMM enriched) with cluster 1. The most up-regulated gene pathways in clusters 2 and 3 related to cell cycle targets of E2F transcription factors and MYC proliferation pathways. The most down-regulated gene pathways in clusters 2 and 3 were IFN-gamma, IFN-alpha and TNF-alpha response and signalling.
Conclusion:
Changes in the cellular iTME mirror the disease course better than changes in the malignant clone or humoral iTME. Patients with more refractory MM have a smaller pool of naïve T cells which express TIGIT or CD127 and could be "revived" with anti-TIGIT antibodies or IL-7 prior to manufacturing CART cells or administering BCMA-based therapies. Significant heterogeneity exists within the more refractory subgroups, with some patients having more dysfunctional T cell subsets which may be less responsive to immunotherapeutic approaches. The malignant transcriptome of samples in clusters 2 and 3 parallels the aggressive clinical course, with myc upregulation and downregulation of cytokine pathways that mediate an antitumor immune response. This study suggests that the MM iTME becomes more dysfunctional with therapy and may explain the differential sensitivity of patients to immunotherapeutic approaches.
Kumar:MedImmune: Research Funding; Janssen Oncology: Other: Research funding for clinical trials to the institution, Consulting/Advisory Board participation with no personal payments; BMS: Consultancy, Research Funding; Tenebio: Other, Research Funding; Genecentrix: Consultancy; Sanofi: Research Funding; Genentech/Roche: Other: Research funding for clinical trials to the institution, Consulting/Advisory Board participation with no personal payments; Oncopeptides: Consultancy, Other: Independent Review Committee; IRC member; Adaptive Biotechnologies: Consultancy; Takeda: Other: Research funding for clinical trials to the institution, Consulting/Advisory Board participation with no personal payments; Merck: Consultancy, Research Funding; AbbVie: Other: Research funding for clinical trials to the institution, Consulting/Advisory Board participation with no personal payments; Dr. Reddy's Laboratories: Honoraria; Amgen: Consultancy, Other: Research funding for clinical trials to the institution, Consulting/Advisory Board participation with no personal payments, Research Funding; Carsgen: Other, Research Funding; Novartis: Research Funding; Cellectar: Other; Kite Pharma: Consultancy, Research Funding; Karyopharm: Consultancy; Celgene/BMS: Other: Research funding for clinical trials to the institution, Consulting/Advisory Board participation with no personal payments.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal